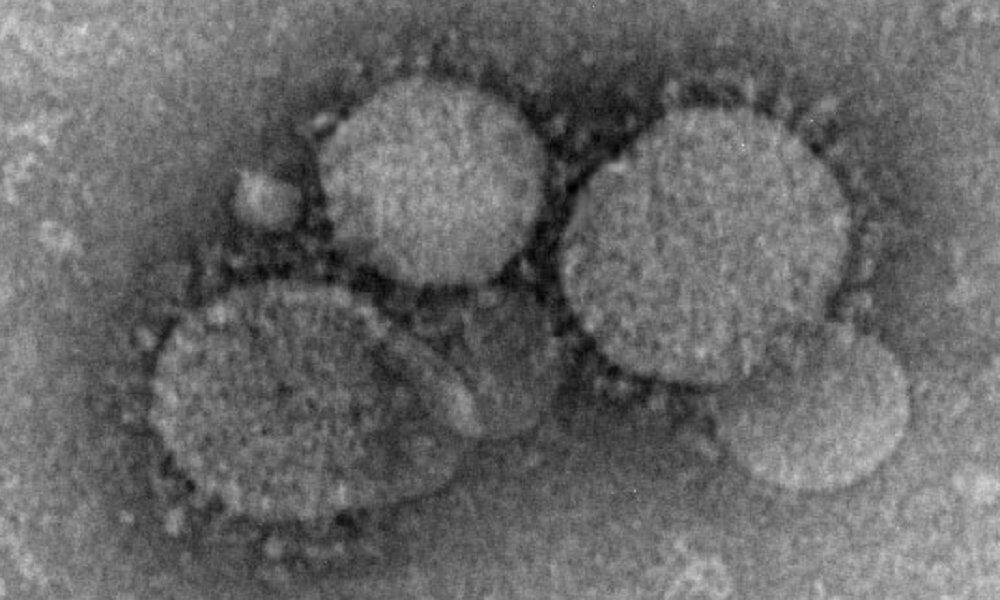
The French Ministry of Health has confirmed two cases of Middle East Respiratory Syndrome coronavirus (MERS-CoV) in individuals who recently traveled to the Arabian Peninsula. Following symptom development, both patients were hospitalized for precaution and are currently in stable condition. Contact tracing, testing, and isolation measures are underway to limit potential transmission, though no secondary spread has been detected within France. MERS-CoV, first identified in 2012, is primarily associated with camels and can cause severe respiratory illness with a high case-fatality rate, as evidenced by past outbreaks like the one in South Korea.
Read the original article here
France confirms 2 MERS coronavirus cases in returning travelers, and it’s definitely a bit of a “wait, what?” moment, isn’t it? After a decade-long absence, MERS is back, and the timing… well, it’s certainly interesting considering all we’ve been through recently. This time, the cases were detected in individuals who had been traveling together in the Arabian Peninsula. Now, that area is known to be a hotspot for MERS, mainly because dromedary camels act as a major reservoir for the virus there. So, the origin isn’t exactly a surprise, but the re-emergence in France certainly is.
Given the history, it’s understandable to have some immediate concerns. MERS, or Middle East Respiratory Syndrome, is a serious illness, and it’s important to remember that it has a significantly higher mortality rate than COVID-19. While COVID had a case mortality rate of around 1% (though some argue that’s an overestimation), MERS can reach a staggering 30%. That’s a huge difference, making it a potentially much deadlier threat. Of course, the flip side is that, thankfully, MERS isn’t known for spreading easily between people outside of close contacts or hospitals. That’s a crucial distinction, because it means that even though it’s deadly, it’s not as readily transmissible as something like COVID.
But here’s where things start to get really concerning: the potential for recombination. Viruses, as we know, can sometimes swap genetic material if they infect the same cell. We’ve seen it with influenza, where different strains mix and create new variants. And the real worry is that MERS could potentially recombine with COVID. While they share a genus, and can recombine if present in the same cell at the same time, this creates a potential for a super-charged virus that’s both highly contagious and potentially much more lethal. Frankly, that’s the stuff of nightmares.
The good news, and there is some, is that there are companies actively working on MERS vaccines. We’ve seen some impressive advancements in vaccine development, particularly in response to COVID, so there’s hope that we could have defenses in place if MERS were to become a bigger threat. In the meantime, proper testing and tracing are absolutely crucial. This is how authorities manage to identify and isolate cases, minimizing the risk to the wider population. The emphasis on testing and tracing is vital, as it’s the first line of defense in containing the virus. It allows authorities to quickly identify and isolate cases, limiting the virus’s spread.
It is worth noting that MERS has been around for a while. The first cases popped up in 2013. However, the transmission rates, especially outside of close contact or hospital environments, have been limited. So, it never quite achieved the kind of widespread pandemic status that we saw with COVID-19. In comparison to Covid, which spread fast, MERS historically has not.
Of course, the fear of the unknown is always a factor in these situations. But the lessons we’ve learned from COVID could also be a major asset. Global health systems are now much better equipped to handle infectious diseases, having gone through the unprecedented experience of COVID-19. If MERS were to gain a foothold, we’d be better prepared, with quicker response times, more testing capacity, and possibly even preventative measures like vaccines.
The situation in Korea provides a cautionary tale. They were particularly vigilant about COVID, having learned a hard lesson from earlier outbreaks of SARS and MERS. The historical context shows that past experiences shape how countries react. That’s why every government needs a strong response plan.
It is also worth mentioning that dromedary camels likely encountered SARS-CoV-2. So, while things have been under control since the beginning of the COVID pandemic, it does raise some questions about the potential for future cross-species transmission or recombination events.
Ultimately, while the return of MERS is definitely something to take seriously, it’s not necessarily a reason to panic. The situation needs to be carefully monitored. The potential for the virus to change is something to be aware of. But the fact that public health is now equipped with more knowledge, experience, and tools puts us in a better position than we were just a few years ago. Hopefully, the world can avoid a repeat of the chaos we saw with COVID-19.