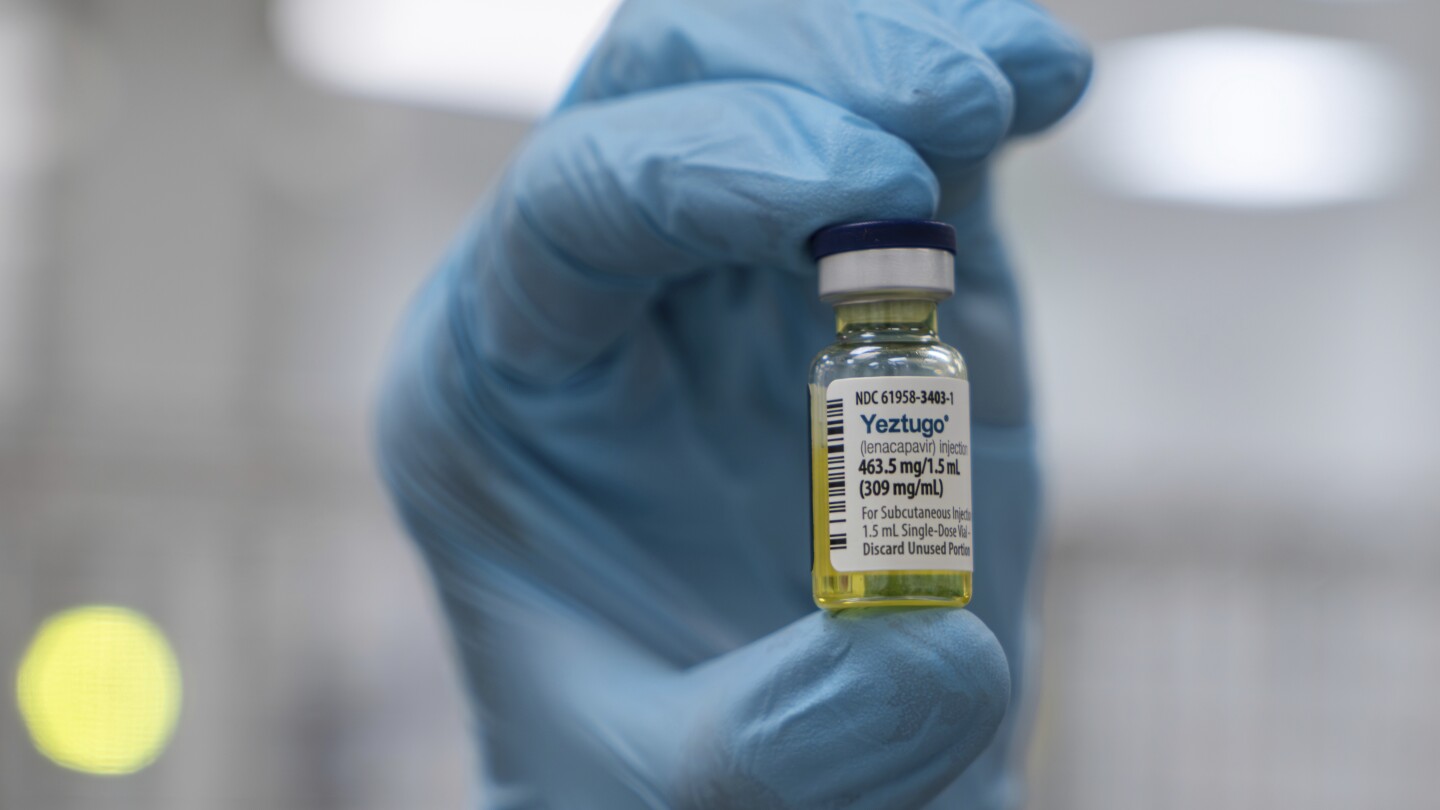
The U.S. has approved lenacapavir (Yeztugo), a twice-yearly HIV prevention injection, marking a potential global breakthrough. Highly effective in clinical trials, reducing new infections nearly to zero in some groups, it offers a longer-lasting alternative to daily PrEP pills. However, access remains a concern due to U.S. healthcare funding cuts and global disparities, potentially limiting its impact despite Gilead’s efforts to provide low-cost versions in some countries. The high initial price also poses a challenge to widespread adoption.
Read the original article here
The FDA’s approval of a twice-a-year injection to prevent HIV is undeniably a monumental achievement in the fight against the virus. This groundbreaking development offers a significant improvement over existing preventative measures, promising a more convenient and potentially more accessible way to protect against HIV infection. The potential for widespread impact is vast, marking a turning point in global public health.
However, the excitement surrounding this medical breakthrough is tempered by concerns regarding equitable access. While the scientific hurdle has been overcome, the challenge now lies in ensuring that this life-saving medication reaches those who need it most. The rollout faces potential obstacles related to funding, healthcare infrastructure, and geographical limitations. The dream of widespread availability might be hampered by realities of unequal distribution.
The convenience of a twice-yearly injection is a compelling advantage compared to the daily pill regimens currently available as pre-exposure prophylaxis (PrEP). This shift could significantly improve adherence rates, as the less frequent dosing reduces the burden on individuals and minimizes the potential for missed doses. This is particularly important considering the long-term commitment required for effective HIV prevention.
The discussion around the classification of this injection also highlights the nuances of medical terminology. While it functions similarly to a vaccine in preventing infection, it isn’t a vaccine in the strictest sense. It’s more accurately categorized as PrEP, working by interfering with the HIV virus’s life cycle rather than stimulating the body’s immune response. This distinction is crucial for accurate communication and public understanding.
The relatively infrequent dosage—twice a year—is a stark contrast to daily PrEP pills, potentially leading to increased uptake. This approach might be particularly appealing to individuals who struggle with daily pill adherence due to lifestyle, logistical, or psychological factors. The convenience factor alone could represent a significant step towards increasing the effectiveness of HIV prevention strategies.
Concerns about the cost and potential for profit-driven restrictions on access are legitimate. The high cost of medications is a frequent barrier to access in many healthcare systems, and the potential for pharmaceutical companies to prioritize profit over equitable distribution remains a valid concern. Transparency and affordability must be central to the rollout plan to ensure that this advancement benefits everyone who needs it.
Despite the approval, questions and anxieties surround the regulatory process. The speed of approval, while potentially positive in terms of expedited access, raises some concerns about the thoroughness of testing and regulation. Independent verification from other regulatory bodies, such as the EU, would help bolster public confidence and address any doubts regarding the safety and efficacy of the new injection.
Further complicating the picture is the backdrop of political polarization and misinformation. The approval has become entangled in partisan discussions, with conspiracy theories and unfounded claims circulating online. This underscores the need for clear, factual communication to counter misinformation and ensure that the benefits of this medical advancement are not undermined by political agendas.
In summary, the FDA’s approval of the twice-a-year HIV prevention shot represents a significant scientific triumph. However, the true success of this innovation hinges on overcoming the significant challenges related to equitable access, affordability, and public education. Only by addressing these issues can we fully realize the potential of this medical breakthrough to transform the global fight against HIV. The focus must shift from celebrating the scientific feat to ensuring that this life-saving treatment is accessible to everyone who needs it, regardless of their socioeconomic status or geographical location. The ultimate measure of success will not be the approval itself, but the impact it has on reducing HIV transmission worldwide.