The Trump administration’s budget cuts have eliminated over a dozen CDC data-gathering programs tracking crucial health information, including data on abortions, lead poisoning, sexual violence, and youth smoking. These cuts, justified as eliminating waste and focusing on infectious diseases, have left health experts concerned about a lack of crucial data for understanding and addressing public health issues. The resulting data gaps hinder the ability to monitor disease trends and effectively combat health threats, raising concerns about the administration’s commitment to comprehensive health surveillance. While the National Center for Health Statistics remains largely intact, the loss of numerous other programs significantly impairs the nation’s ability to track and understand various health problems.
Read the original article here
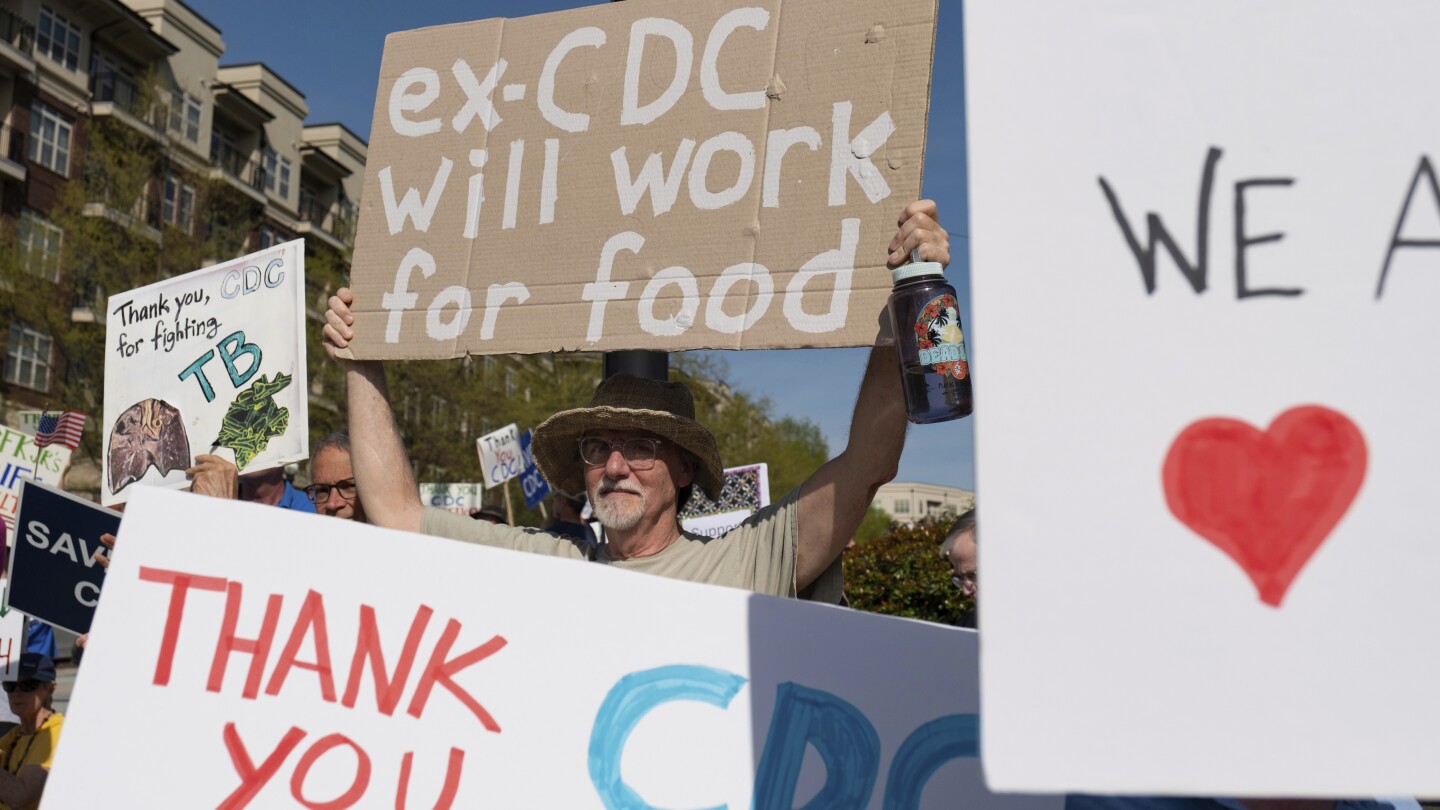
Cuts have eliminated more than a dozen US government health-tracking programs, a development that raises significant concerns about the nation’s ability to monitor and address critical public health issues. The Centers for Disease Control and Prevention (CDC), a key agency in this effort, has seen the termination of programs monitoring a wide range of health concerns.
Cuts have eliminated crucial programs focused on vulnerable populations, notably women, youth, and workers. Among the terminated programs, experts at the CDC were tracking abortions, pregnancies, job-related injuries, lead poisonings, sexual violence, and youth smoking. The elimination of these data-gathering initiatives raises serious questions about the government’s commitment to addressing these vital health challenges.
Cuts have potentially undermined the effectiveness of agencies beyond the CDC. The elimination of job-related injury tracking, for instance, could significantly weaken the Occupational Safety and Health Administration (OSHA), making it harder to enforce workplace safety regulations. Without reliable data on workplace injuries, it becomes difficult to identify trends, hold employers accountable, and implement effective preventative measures.
Cuts have created a situation where the lack of data could be used to justify further cuts or deregulation. By eliminating the record of workplace injuries, it becomes easier to deny or minimize the negative impact of weakening or eliminating OSHA. This is a concerning pattern, where data itself is used as a tool to dismantle essential public health protections.
Cuts haven’t necessarily eliminated all tracking entirely. While the termination of CDC programs is a setback, many medical groups independently run their own registries and tracking systems for local populations. These systems often utilize automated methods, meaning the complete cessation of data collection isn’t guaranteed. However, the loss of centralized, nationally coordinated data collection significantly diminishes the scope and effectiveness of public health monitoring.
Cuts represent a broader philosophical shift in how public health is viewed. The elimination of these programs suggests a lack of priority placed on comprehensive health surveillance. The implied logic behind such decisions might be interpreted as a belief that resources are better allocated elsewhere, or perhaps even a disinterest in tracking health issues at all. This perspective, reminiscent of previous administrations’ approaches to data related to COVID-19, raises deep anxieties about the future of public health in the US.
Cuts also pose a challenge in data continuity and expertise. The abrupt termination of these programs likely resulted in a loss of institutional knowledge and experienced personnel. When the individuals responsible for analyzing and interpreting the data are dismissed, there’s a significant risk of data discontinuity. It may take considerable time and effort to rebuild expertise and re-establish effective data collection and analysis, even if the programs were eventually reinstated. The loss of this expertise creates a significant gap in the public health response.
Cuts highlight the dangers of electing officials who prioritize short-sighted policies over evidence-based decision-making. The elimination of these critical health-tracking programs is a direct consequence of policy choices that prioritize ideology or short-term gains over long-term public health. The impact of these cuts will be felt for years to come, potentially exacerbating health disparities and undermining the nation’s ability to respond effectively to public health crises.
Cuts have undermined public trust and transparency. The questionable justifications for these cuts, combined with the lack of transparency surrounding the decision-making process, only serve to further erode public trust in government institutions. This loss of trust is detrimental to public health, hindering efforts to promote health literacy and encourage public cooperation in disease prevention and control initiatives.
In conclusion, the elimination of more than a dozen US government health-tracking programs represents a significant blow to the nation’s ability to effectively monitor and address public health challenges. The impacts extend beyond the immediate loss of data, affecting vulnerable populations, weakening regulatory agencies, creating data gaps, and undermining public trust. Addressing these shortcomings requires a renewed commitment to data-driven decision-making, resource allocation, and transparency in public health policy.