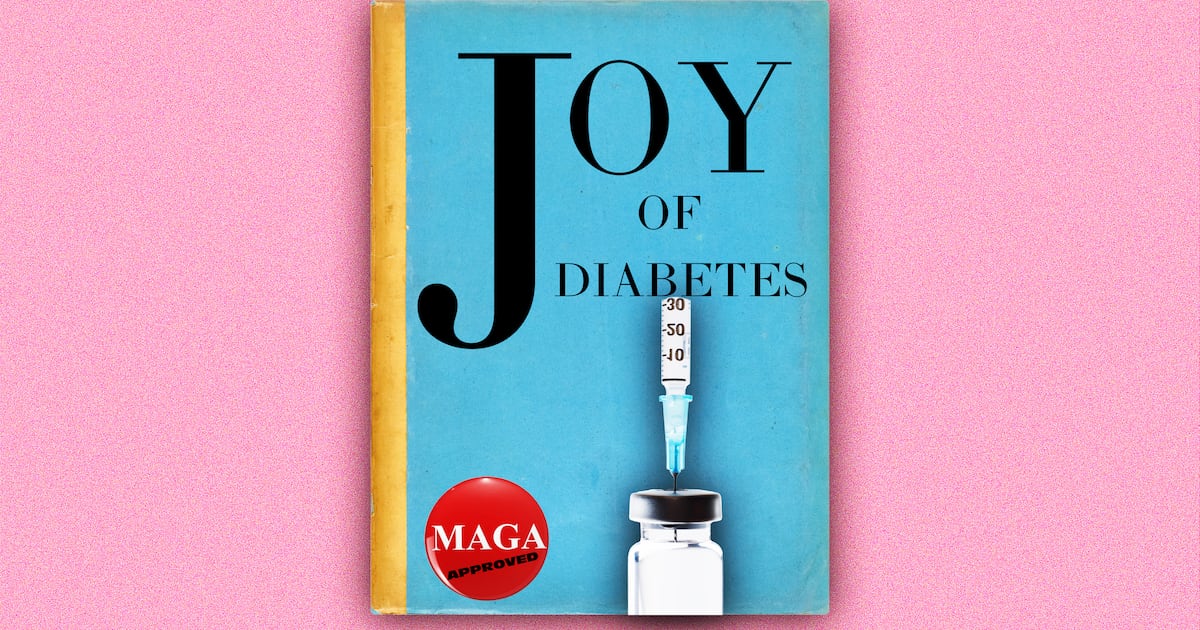
FDA Commissioner Marty Makary controversially suggested that cooking classes might be a more effective diabetes treatment than insulin alone, despite overwhelming scientific evidence supporting insulin’s safety and efficacy. This statement promotes a report from the Trump administration’s “Make America Healthy Again” commission, which advocates for a proactive healthcare system. However, the commission, led by Robert F. Kennedy Jr., has faced criticism for promoting unsubstantiated claims regarding vaccines, fluoride, and food dyes. Makary’s remarks thus align with a broader initiative criticized for prioritizing unproven approaches over established medical consensus.
Read the original article here
RFK Jr.’s proposed solution to the diabetes crisis—cooking classes over insulin—is deeply concerning and fundamentally misunderstands the nature of the disease. Type 1 diabetes, an autoimmune disorder, necessitates insulin for survival. Cooking classes, while beneficial for managing blood sugar levels in both type 1 and type 2 diabetes, cannot replace the vital role of insulin in regulating blood glucose. This approach ignores the basic science of the disease and demonstrates a dangerous disregard for the well-being of millions.
This suggestion is not merely misguided; it’s potentially lethal. Denying people access to life-saving medication based on a belief that dietary changes alone can suffice is reckless and irresponsible. For individuals with type 1 diabetes, insulin is not a matter of lifestyle choice; it’s a physiological necessity. Without it, severe complications, including diabetic ketoacidosis (DKA) and death, can swiftly follow. The idea of substituting cooking instruction for insulin therapy is akin to recommending kale in place of a leg cast for a broken bone.
The inherent danger of this policy is further amplified by the potential for misinterpretation and misinformation. Many individuals, especially those already distrustful of mainstream medicine, may be swayed by this proposal, choosing to forgo insulin treatment based on the perceived endorsement from a high-ranking official. This is particularly worrying given the existing challenges in accessing affordable healthcare and the prevalence of misinformation online. The consequence could be avoidable deaths and long-term health complications for many.
Moreover, suggesting cooking classes as an alternative to insulin highlights a callous disregard for the complexities and challenges of managing diabetes. Individuals struggle with navigating the complexities of meal planning, ingredient selection, and maintaining consistent blood sugar control, even with proper medical care. While healthy eating and regular exercise are essential components of diabetes management, they are supplementary measures, not substitutes for essential medication.
This proposal seems to indicate a broader trend of prioritizing ideological agendas over evidence-based healthcare. It reflects a dangerous pattern of downplaying the efficacy of proven medical interventions in favor of unproven alternative approaches. The lack of scientific basis supporting this suggestion points to a concerning detachment from medical expertise and a troubling dismissal of the lived experiences of those affected by this disease. The comparison to historical instances of medical negligence and eugenics is disturbing and underscores the gravity of this situation.
The emotional toll on those affected by this proposal is immense. Diabetics already face immense physical and emotional burdens in managing their condition, and this misguided suggestion adds insult to injury. The frustration and fear are palpable, fuelled by the feeling of being disregarded and disrespected by those in positions of power. The sheer absurdity of the proposal—a cookbook as a replacement for insulin—only exacerbates the sense of despair and outrage.
The lack of understanding regarding the fundamental differences between type 1 and type 2 diabetes further emphasizes the troubling lack of medical expertise driving this suggestion. Type 2 diabetes, often linked to lifestyle factors, can sometimes be managed with dietary changes and exercise. However, type 1 diabetes requires life-long insulin treatment; this is not a matter of choice or lifestyle modification. To conflate the two is a dangerous oversimplification that risks serious consequences.
The current state of affairs points to a deep-seated problem within our healthcare system, a problem that goes beyond just this specific suggestion. The ease with which such an inaccurate and potentially harmful idea can be put forth highlights a larger crisis of misinformation, political maneuvering, and a detachment from medical evidence. The potential for widespread harm stemming from this proposal is undeniable and demands immediate and decisive action to correct the course. A shift toward evidence-based healthcare and a respectful approach to the complex challenges of managing chronic diseases is urgently needed.