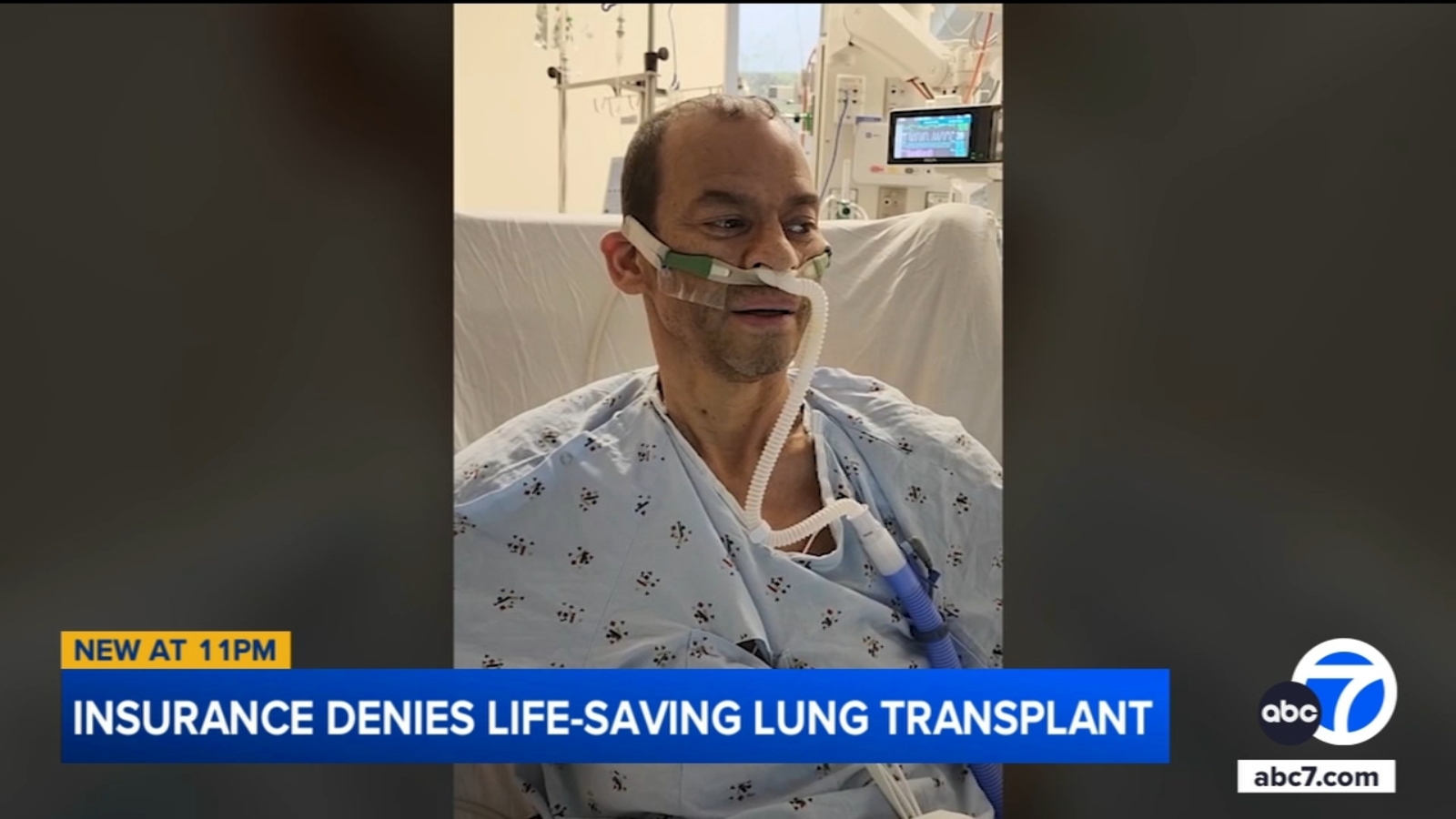
Deron Wells, a 59-year-old father of three with stage 4 lung cancer, had his double-lung transplant coverage denied by Cigna despite prior approval for the procedure and transfer to Northwestern Medicine in Chicago. His insurance company cited coverage guidelines based on national clinical standards, while his family and friends are actively campaigning for his appeal. The denial occurred just as he was preparing for travel, leaving his life hanging in the balance. Wells awaits a Thursday decision on his appeal, clinging to hope for a life-saving transplant.
Read the original article here
Cigna denies a man a life-saving lung transplant shortly before his scheduled operation, a decision sparking outrage and highlighting the complex issues surrounding healthcare access and affordability in the United States. This situation throws into sharp relief the stark contrast between the immense profits generated by insurance companies and the devastating consequences for individuals denied crucial medical care. The sheer callousness of the decision, especially given the patient’s advanced stage of lung cancer, underscores the ethical dilemmas inherent in a for-profit healthcare system.
The man, already battling stage 4 lung cancer, was on the verge of receiving a double-lung transplant – a procedure offering a potential, albeit not guaranteed, extension of his life. However, this hope was cruelly dashed when Cigna, his insurance provider, denied coverage, leaving him facing a grim reality. The timing of the denial, mere moments before the scheduled operation, adds another layer of cruelty to this already devastating situation. It’s not just a question of money; it’s about the brutal destruction of hope at the eleventh hour.
The incident is indicative of a larger problem within the American healthcare system – the financial burden of medical care. While other developed nations grapple with issues like wait times, the US unique challenge is the pervasive fear of financial ruin. This anxiety pervades every aspect of healthcare decisions, from preventative care to life-saving treatments. The sheer cost of healthcare, coupled with the opaque and often arbitrary decision-making processes of insurance companies, contributes to this crippling fear. The potential for bankruptcy from a medical emergency is a very real fear for many Americans, and this case exemplifies the extreme end of that fear.
The financial disparity is striking. While Cigna boasts profits of $1.3 billion in a single quarter of 2025, a figure that underscores their financial health, this man is denied a chance at life. The CEO’s exorbitant compensation package further exacerbates the public’s anger, suggesting a stark disconnect between corporate greed and individual well-being. This disconnect fuels the perception that these companies prioritize profit over human life, and cases like this only intensify that perception.
Questions have been raised regarding the nature of the transplant as part of a clinical trial. While some argue that insurance companies typically don’t cover experimental treatments, the urgency of the situation and the patient’s dire condition warrant further scrutiny. The fact that the man’s life was deemed less valuable than the cost of the procedure is a damning indictment of the current healthcare system’s priorities. It’s important to remember that clinical trials often involve experimental components but aim to improve treatments available to future patients. The argument for excluding the cost of this particular treatment from insurance coverage is, therefore, debatable and subject to a variety of interpretations.
There are legitimate questions surrounding the medical aspects of this case. The efficacy of a double-lung transplant for stage 4 lung cancer is undoubtedly complex. The advanced stage of the cancer and the required immunosuppressants post-transplant present considerable challenges. While there’s a chance it could prolong life, the chance of success in this situation is admittedly lower than many other medical scenarios. The question remains, however, whether the insurance company should bear the full cost of this experimental treatment, or whether the responsibility falls elsewhere, especially in light of the clinical trial context.
This incident prompts intense debate regarding for-profit healthcare. The blatant profit motive of insurance companies and their role in life or death decisions remains the key point of contention. The sheer lack of transparency in these companies’ decisions fuels distrust. It also fuels public outrage at a system that prioritizes profit margins over human well-being. The comments about “death panels” and other criticisms reflect the public sentiment that the system is inherently flawed, and cases like this only reinforce the sentiment.
Ultimately, the case highlights a systemic failure. The lack of transparency, the exorbitant costs, and the prioritization of profit over human life are all contributing factors. The outrage is justified, and it calls for a critical re-evaluation of the US healthcare system. The public needs to demand greater accountability and transparency from insurance companies and advocate for healthcare reform that prioritizes the well-being of individuals over profit. This is not simply an isolated case; it’s a symptom of a much larger, deeply entrenched problem. The question remains: how many more lives will be sacrificed at the altar of corporate profit before real change occurs?