Ontario is currently experiencing a significant measles outbreak, one of the province’s largest in recent history. The surge in cases highlights the importance of vaccination. Public health officials are urging Ontarians to check their immunization status and ensure they are up-to-date on their MMR vaccine. This outbreak underscores the ongoing need for robust vaccination programs to prevent the spread of preventable diseases.
Read the original article here
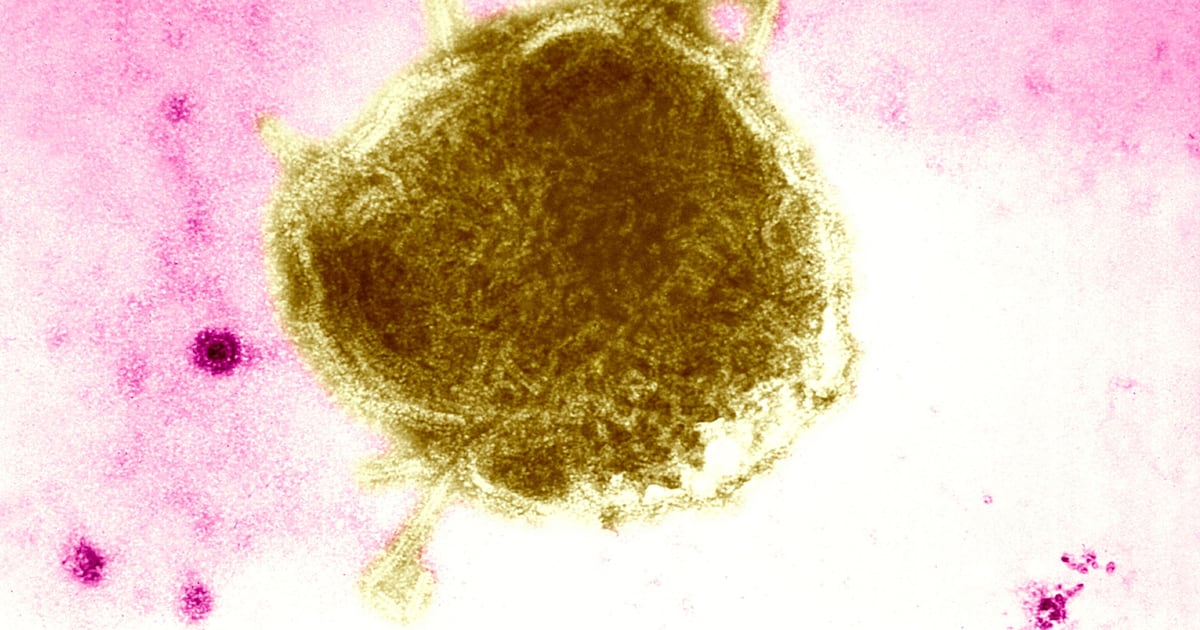
Ontario is currently grappling with one of its largest measles outbreaks in recent history. This surge in cases is particularly concerning, given that measles is a highly contagious disease that can lead to serious complications, even death. The situation highlights the crucial importance of vaccination and underscores the potential consequences of declining vaccination rates.
The current outbreak appears to be linked to a significant drop in measles vaccination rates. While historical vaccination rates in Ontario were high, consistently around 85-90%, the pandemic appears to have significantly impacted this figure. A considerable decrease to around 40% has been reported, although this figure seems to be inaccurate compared to nationwide data. Even adjusted national data reveals a concerning drop from pre-pandemic levels of around 89% to roughly 83% in 2022 and 2023. Regardless of the precise Ontario figure, the decline in vaccination, whether statewide or localized to specific communities, is undeniably contributing to the outbreak.
This decline isn’t solely attributable to any single factor. While anti-vaccine sentiments undoubtedly play a role, mirroring trends in other parts of the world, the disruption caused by the pandemic is a significant contributor. Many parents postponed or missed routine childhood vaccinations due to school closures, limited access to healthcare services, and general pandemic-related anxieties. This lapse in routine immunizations has left a considerable portion of the population vulnerable to measles infection.
The spread is particularly concentrated within specific communities. Reports suggest a higher concentration of cases among unvaccinated individuals within certain religious communities, such as Anabaptist and Calvinist groups, who often maintain their own independent schools. This pattern underscores the necessity of targeted public health interventions within these communities to promote vaccination and prevent further transmission.
The situation raises important questions about public health policy and enforcement. While school boards generally require proof of vaccination, the enforcement seems inconsistent, allowing exemptions based on personal beliefs. This lack of strict adherence to vaccination mandates, coupled with the low vaccination rates, has created fertile ground for the virus to spread rapidly. This issue highlights a crucial dilemma: balancing individual liberties with the collective health of the population.
The concern extends beyond the immediate threat of measles. The outbreak serves as a stark reminder of the fragility of herd immunity and the potential for easily preventable diseases to re-emerge when vaccination rates decline. The experience of other regions, notably the United States, where similar outbreaks have occurred due to pockets of low vaccination rates, highlights the potential for widespread contagion.
The current situation emphasizes the need for a multi-pronged approach to address the measles outbreak. This includes not only increased efforts to promote vaccination but also improved enforcement of vaccination mandates in schools and other public settings. Public health campaigns should focus on dispelling misinformation and providing accurate, accessible information about the safety and efficacy of vaccines. Furthermore, addressing systemic barriers to vaccination access, such as financial constraints or logistical challenges, is vital in ensuring equitable protection for all members of the community.
The current measles outbreak in Ontario is a serious public health concern, demanding immediate and decisive action. It’s a complex issue with no easy solution, but addressing the underlying causes—low vaccination rates and inconsistent enforcement of vaccination policies—is crucial in containing the current outbreak and preventing future ones. The situation underscores the importance of prioritizing preventative measures, such as routine vaccinations, in safeguarding community health. The conversation surrounding this outbreak also highlights the need for a more nuanced discussion on public health policy, balancing individual autonomy with the collective good.