A new study reveals that the Huntington’s disease mutation, while present from birth, remains harmless for decades. The mutation gradually expands, increasing the number of CAG repeats in a specific gene. Once the repeat count surpasses approximately 150, a threshold is reached, triggering the production of toxic proteins and subsequent neuron death. This neuronal degeneration accounts for the disease’s characteristic symptoms, which typically manifest between ages 30 and 50. These findings suggest that inhibiting the expansion of CAG repeats may be a more effective therapeutic strategy than targeting the toxic protein itself.
Read the original article here
Huntington’s disease, a devastating and fatal brain disorder, has long been linked to a specific genetic mutation. However, the mystery of why individuals with this mutation from birth often don’t develop symptoms until much later in life has puzzled scientists for years.
This new research provides a surprising answer: the initial mutation appears to be relatively harmless for an extended period. Instead of immediately causing problems, it slowly and quietly grows into a larger, more significant mutation.
This gradual expansion continues until it reaches a critical threshold. Once this point is reached, the process generates toxic proteins, initiating cellular damage and ultimately leading to cell death in the affected areas of the brain. This explains the delayed onset of symptoms.
The disease’s impact is profoundly heartbreaking. Many accounts depict the devastating effects on families, watching loved ones – children, siblings, parents – slowly lose their physical and cognitive abilities, their personalities altered by the relentless progression of the disease. The shared experience of loss and grief, coupled with the knowledge of the disease’s heritable nature, creates a profound sense of helplessness and despair.
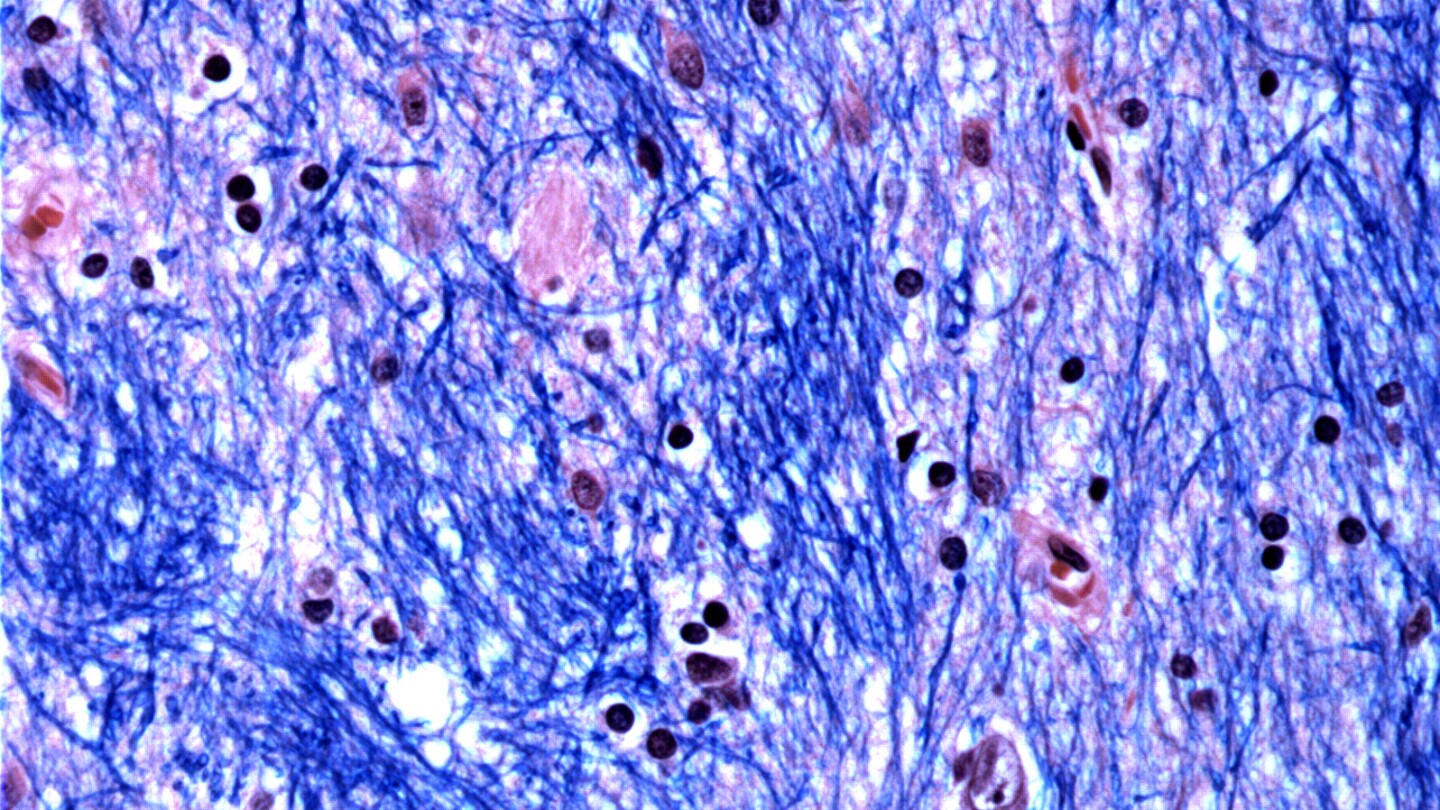
The underlying biological mechanisms involved in the mutation’s growth and the subsequent cellular toxicity are complex and fascinating. The Huntington gene (HTT) contains repeating elements in its DNA sequence, specifically CAG trinucleotide repeats. The process of turning this DNA into RNA for protein production involves unwinding and separating the DNA strands. During this process, the DNA can misalign, due to the long CAG repeats, creating loop structures recognized as errors by the cell’s DNA repair mechanisms.
It’s these repair attempts that sometimes lead to an expansion of the CAG repeats, inadvertently amplifying the mutation over time. The accumulation of these expanded repeats results in the production of an abnormally long and toxic form of the huntingtin protein. This altered protein disrupts normal cellular function, ultimately causing the neuronal damage characteristic of Huntington’s disease.
Despite the discovery of the huntingtin protein over 30 years ago as the causative agent of HD, its precise molecular function in healthy cells remains elusive. Current research focuses on understanding the protein’s cellular interactions and how these interactions become dysfunctional in HD, potentially leading to effective treatment strategies.
The possibility of gene editing therapies, such as CRISPR, offers a glimmer of hope. CRISPR’s ability to precisely target and modify specific DNA sequences makes it an attractive tool for correcting the expanded CAG repeats in the HTT gene. However, practical challenges remain, primarily the need for efficient delivery of CRISPR technology across the blood-brain barrier to reach the affected brain cells.
While targeting these repeating sequences with CRISPR seems straightforward – conceptually, like a “CTRL-F” for repeating DNA segments – the actual implementation is challenging. The length of the repeat sequences and the potential for misalignment during DNA replication complicate the precise targeting and removal of the problematic repeats. The potential for off-target effects also needs careful consideration.
This new understanding of the disease’s progression offers a pathway towards developing new treatments. Further research into the cellular mechanisms and the precise nature of the toxic huntingtin protein is crucial. This includes investigating whether the mechanisms are applicable to other similar neurodegenerative diseases, offering broader implications for treatment development.
The personal accounts shared highlight the urgent need for further research and effective treatments. The suffering caused by Huntington’s disease underscores the importance of continued scientific pursuit, not just for a cure, but also for the development of effective therapies to slow or halt the progression of the disease. The possibility of gene therapy, along with ongoing research, offers hope for a brighter future for those affected by this devastating illness.