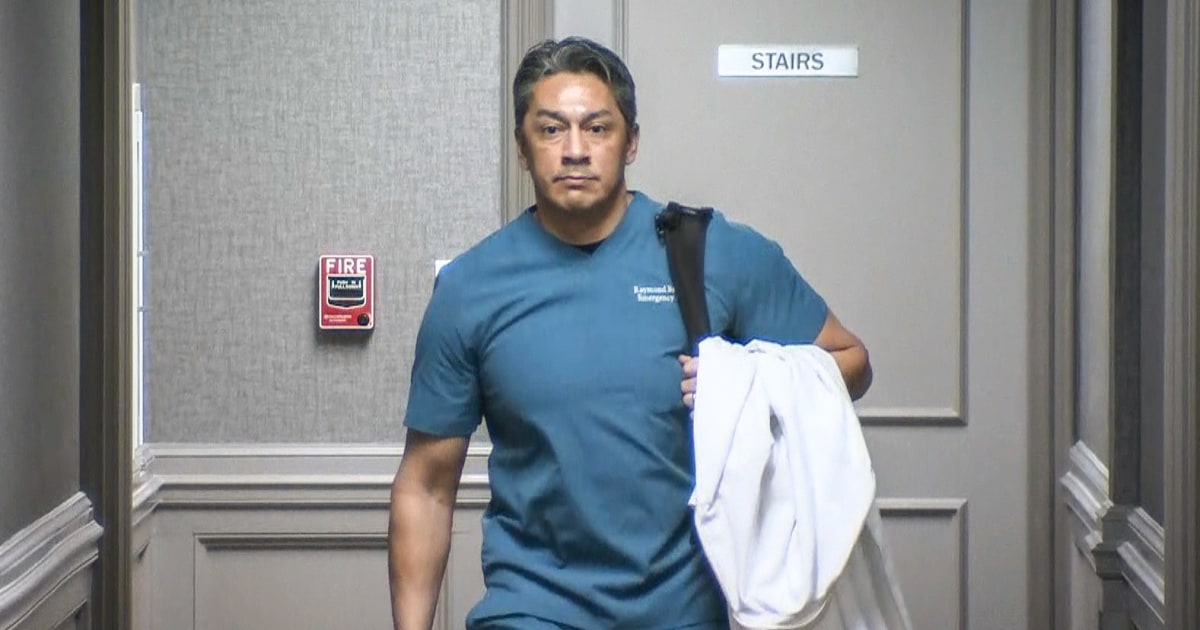
This article details the case of Dr. Ray Brovont, an emergency room physician fired after repeatedly raising concerns about unsafe staffing levels at Overland Park Regional Medical Center, exacerbated by the hospital’s expansion. His dismissal highlights a growing problem within for-profit emergency department management, where profit prioritization allegedly compromises patient safety. Brovont’s lawsuit against EmCare, later acquired by Envision Healthcare, resulted in a significant financial award, exposing the company’s practices of circumventing state laws prohibiting corporate practice of medicine through shell physician ownership. The case underscores the conflict between profit motives and patient care in the increasingly prevalent for-profit model of emergency department staffing.
Read the original article here
The recent firing of an emergency room doctor for raising concerns about insufficient staffing levels shines a harsh light on the detrimental effects of for-profit firms on U.S. healthcare. The doctor’s dismissal, reportedly due to financial motivations prioritizing profits over patient care, highlights a disturbing trend where corporate interests overshadow the well-being of patients and medical professionals alike.
This isn’t an isolated incident. The pressure to meet stringent metrics and avoid penalties for exceeding allotted patient time creates a system where rushed care becomes the norm, impacting the quality of treatment received. The financial burdens placed on physicians, such as the $3,000 fine levied on a doctor for spending extra time with a patient, incentivize speed over thoroughness, a dangerous dynamic within a profession demanding meticulous attention to detail.
The consequences extend beyond individual doctors. The pervasive influence of for-profit entities is transforming the healthcare landscape, altering the very fabric of patient care. Hospitals, once primarily focused on patient well-being, are now increasingly beholden to shareholder demands, resulting in understaffing, cost-cutting measures, and a decline in the overall quality of services provided.
This trend is not limited to hospitals; it’s spreading rapidly across the veterinary field as well. Private equity firms are aggressively acquiring veterinary practices, driving up prices and jeopardizing access to affordable pet care. This disturbing parallel suggests a wider systemic problem within the healthcare sector, regardless of species.
The issue transcends simple profit maximization; it’s a profound ethical lapse. The statement “Profits are in everyone’s best interest” reflects a cynical disregard for human life, prioritizing monetary gains over the health and safety of those who rely on the system. This prioritization is a stark reminder of the flaws inherent in a for-profit model when applied to a service as critical as healthcare.
The current system lacks sufficient safeguards to protect against this corporate greed. While some regulatory bodies exist, they often seem incapable of effectively addressing the issues. The anonymity afforded to corporate spokespeople further exacerbates the problem, allowing companies to deflect responsibility without accountability.
The impact extends to all levels of healthcare, from emergency rooms to intensive care units. Short-staffing, inadequate resources, and the constant pressure to maximize productivity contribute to a dangerously stressful work environment, negatively impacting patient care and the mental well-being of medical professionals. This leads to burnout, increased error rates, and a reluctance of aspiring medical professionals to enter the field.
The problem’s roots lie in a complex interplay of factors, including the lack of strong regulatory oversight, lobbying efforts by powerful corporations, and public apathy. The common perception of doctors as wealthy and privileged makes it easier for corporate narratives to frame the issue as a conflict between greedy doctors and struggling companies, diverting attention from the crucial role of adequate staffing and resource allocation.
A solution requires multi-pronged approach, involving legislative changes, increased regulatory oversight, and a fundamental shift in societal values. Strengthening regulatory frameworks, empowering unions for medical professionals, and encouraging public discourse about the flaws of the current system are essential first steps towards achieving meaningful change. Ultimately, healthcare should be viewed as a fundamental human right, not a commodity driven by profit.
The crisis facing U.S. healthcare is not simply a matter of economics; it’s a moral imperative. The need for systemic change is undeniable. The current system is failing patients, doctors, and the future of healthcare itself. The time for decisive action is now before the situation deteriorates even further. The question remains: will the necessary changes be implemented before irreparable damage is done? The consequences of inaction are too significant to ignore.